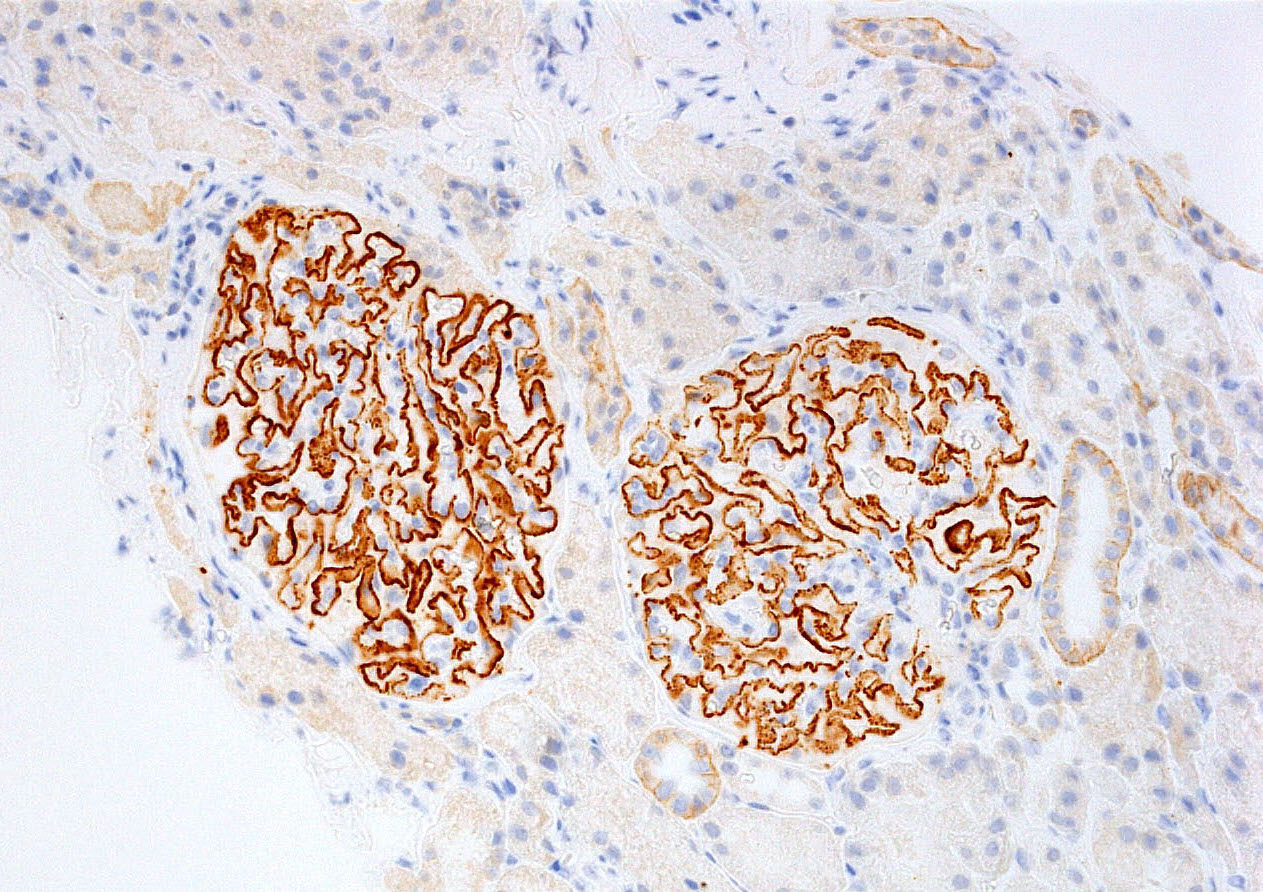
Immunohistochemistry staining for PLA2R
Discovery of autoantibodies against podocyte antigens
In the late 1970s, it became evident that podocyte antigens were targeted by the immune system in patients with primary membranous nephropathy (MN), resulting in subepithelial immune complexes and glomerular injury. It was not until 2009, however, that the major antigen target – M-type phospholipase A2 receptor 1 (PLA2R) – was discovered. PLA2R-associated membranous nephropathy accounts for 70-80% of primary membranous nephropathy cases (Beck et al. 2009 NEJM). Trends in PLA2R antibody titers correlate with proteinuria and changes in antibody levels precede changes in proteinuria by weeks-to-months (Hoxha et al. JASN 2014). The presence of PLA2R antibodies is also associated with developing native membranous nephropathy months-to-years before clinical disease (Burbelo et al. JASN 2020). Hence, the discovery of autoantibodies against podocyte antigens has the potential to revolutionize our approach to diagnosis and treatment for MN patients.
Recently discovered new antigens
Although PLA2R was identified as the main targeted antigen, a substantial proportion of patients still tested PLA2R-negative. In 2014, thrombospondin type 1 domain-containing 7A (THSD7A) was also involved. This antigen represents 1-5% of patients with primary MN. Despite that, antibody titers to TSHD7A are not routinely available in most centers.
Studies on new target antigens in MN showed differences in the characteristics of patients affected and their underlying diseases. Assuming every antigen targeted by autoreactive immune cells represents a subcategory of MN, identifying the involved antigen for every patient can be useful in risk stratifying patients and determining best treatment strategies.
Exostosin 1 and 2 (EXT1/EXT2)-associated MN has a female predominance and were mostly seen in patients with underlying autoimmune diseases such as lupus nephritis. Neural EGF-like-1 protein (NELL1) associated MN mainly presents as primary MN, although a subset of NELL1-associated MN patients (10-33%) have an underlying malignancy.
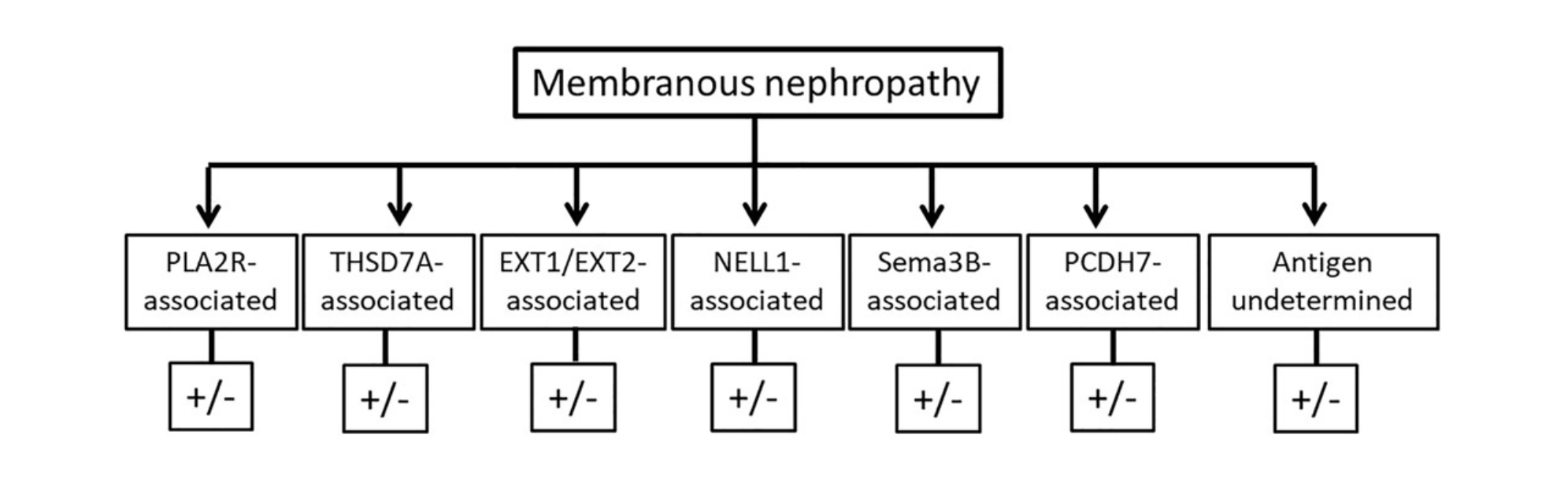
Semaphorin 3B (Sema3B) associated MN is often seen in the pediatric population. Some of these patients have a positive family history for MN, questioning whether a genetic component could be involved. Protocadherin 7 (PHCD7) was another recently discovered antigen associated with MN and is more frequently seeing in the elderly population.
Testing for autoantibodies can pose a challenge, as newly discovered targeted antigens are not clinically available yet. Furthermore, some of them may not be as easily detected in the serum by current testing. EXT1/EXT2 antibodies for example were only visible via pathology staining and not detectable in the serum. For further details on these novel antigens, read a review by Sethi JASN 2021.
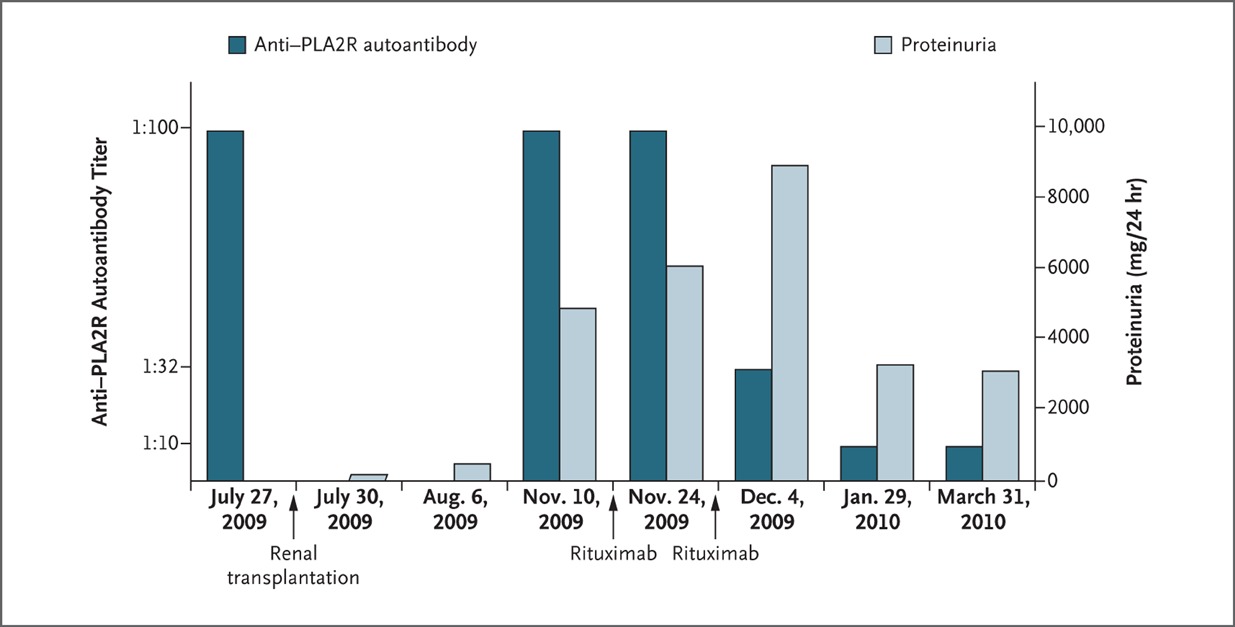
First case study published in NEJM on how serum PLA2R autoantibody levels after transplantation could be associated with recurrent disease and treatment response (Stahl et al. NEJM 2010).
Identifying the key antigen for patients with MN can aid in both the diagnosis and management. We are cautiously optimistic that autoantibody testing and staining will become more important for MN patients in the near future. Of note is that there are many aspects of this noninvasive diagnostic tool that require further investigation. Especially when we look at the transplant population. Most of the research conducted thus far only took PLA2R into account. Nevertheless, various papers are available showing the use of serum PLA2R antibody levels in predicting recurrence after transplant. More on this topic will follow soon in a CJASN review we wrote, highlighting the different diagnostic and management dilemmas transplant physicians face in approaching glomerular disease post-transplantation.